INTRODUCTION
The Medical Society of the State of New York represents tens of thousands of physicians, residents, and medical students across the State, delivering care to patients in small group settings, large group settings, employed by a health system, or in a public health service role. Our diverse membership is committed to ensuring that all New Yorkers have access to quality and affordable physician-led healthcare.
Our efforts to ensure patients receive needed and appropriate care is challenged by an ever-increasing encroachment into care delivery by non-physician providers, health insurers, corporate pharmacy giants, private equity corporations, market-dominant health systems, electronic health record developers and even in some cases policymakers. Their well-intended but sometimes misguided efforts to improve care and reduce costs can have the effect of limiting treatment options for patients, limiting the ability of physicians to advocate for their patients, pushing physicians out of patient care into early retirement or out of the State, or by seeking to replace them altogether with various non-physician providers.
These factors are accelerating the disturbing rise in physician burnout, demoralization and moral injury. As the healthcare landscape continues to rapidly evolve, it is imperative that policymakers recognize and address New York’s notoriously poor practice environment and find solutions that will help improve professional wellbeing and expand patient access to physician-led care.
Statistics continue to show that the overall state of wellbeing for physicians remains disturbingly low. For the fourth year in a row, 60% of physicians report often having feelings of burnout, compared to 40% in 2018.
Moreover, more than half of physicians and medical students know of a physician or colleague who has considered, attempted, or died by suicide.
Nearly 70% of physicians and medical students, and over 60% of medical residents, agree that consolidation in health care is negatively impacting patient access. However, the “Catch-22” is that many physicians believe they have no choice but to practice in large systems as independent practice has become impossible for many due to the enormous and costly infrastructure needed for delivering patient care. This compromises the ability of a physician to be the best advocate for their patients.
One of the driving factors to physician burnout is the overwhelming required use of electronic medical record (EHR) system. For example, between 2022 and 2023, physicians reported an increase of nearly 30 minutes per day in their use EHRs, representing an 8% year-over-year increase. Over half of all physicians indicated that the time they dedicate to EHRs while at home not in their clinical setting is “high” or “excessive.
This is not sustainable, and solutions must be implemented to reverse these problems. For example, 90% of physicians agree that preserving physician autonomy is most helpful as a safeguard against consolidation in healthcare. 79% of physicians and 87% of residents also reported reduction of administrative burdens to be helpful to addressing factors of burnout.
In that regard, policymakers must work to change New York’s notoriously poor practice environment. New York is regularly ranked near the bottom on the list of the best states in which to practice medicine. In part, this has been attributed to a lack of competitive compensation, excessive regulatory requirements, and exorbitant liability costs. This is exacerbated by the pervasive cuts in the Medicare fee schedule, which often forms the basis for commercial health insurance reimbursement. New York has already lost countless physicians to early retirement or to other states with practice environments more welcoming to physicians. Furthermore, according to studies, New York retains less than half of the physicians it pays to train.
These trends must change. Replacing physicians with less skilled non-physicians is not the panacea. We cannot ensure meaningful access to care for patients unless we work to ensure that we have an available supply of primary and specialty care-trained physicians to meet patient needs. MSSNY’s 2025 Legislative Program sets forth several initiatives to help support maintaining and increasing physician supply in regions across the State.
THE NEED FOR HEALTH PAYER REFORMS
Legislation and other policy changes are needed to counteract pervasive health insurer-imposed administrative barriers that interfere with patient care delivery and needlessly delay fair payment for care delivered to patients.
Insurers can impose these burdens because of their market dominance. According to the 2023 AMA Competition in Health Insurance Competition in Health Insurance: A comprehensive study of U.S. Markets, in most regions of New York there are just two insurers that collectively control nearly half (44%) of the regional market.1 Physicians must either accept insurers’ terms or impelled to join large health systems in order to stay in business and continue to deliver patient care in the communities they serve.
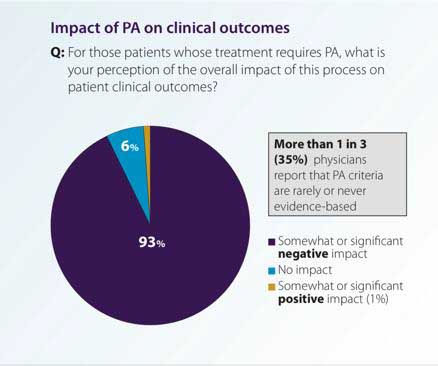 One of the significant impacts of market dominance by insurers is through needlessly complicated prior authorization (PA) policies. According to an American Medical Association (AMA) study released in the spring of 2023, 94% of physicians surveyed reported care delays due to PA hassles and 78% said that PA can lead to patients abandoning their treatments. Moreover, 93% reported that excessive prior authorization burdens have had a negative impact on clinical outcomes, while 53% of the physicians surveyed said that PA had interfered with a patient’s ability to perform their jobs.
One of the significant impacts of market dominance by insurers is through needlessly complicated prior authorization (PA) policies. According to an American Medical Association (AMA) study released in the spring of 2023, 94% of physicians surveyed reported care delays due to PA hassles and 78% said that PA can lead to patients abandoning their treatments. Moreover, 93% reported that excessive prior authorization burdens have had a negative impact on clinical outcomes, while 53% of the physicians surveyed said that PA had interfered with a patient’s ability to perform their jobs.
To counteract the disproportionate market power of insurers, MSSNY supports the following important reforms in the upcoming New York State
legislative session.
Collective Negotiations. Legislation is needed to allow independently practicing physicians to collectively negotiate contract terms, including administrative processes such as prior authorizations (PAs), with insurance companies. This will enable physicians to better advocate for their patients by pushing back against policies that delay access to care that insurers use to guarantee profits. Reduced administrative burdens will also save physician practices time and costs that can ultimately be spent caring for patients.
Prior Authorization Reform. The Legislature took some modestly positive steps in the 2024 Legislative Session to reduce some of the hassles caused by step therapy medication protocols and Workers Compensation care delays. However, these steps barely begin to address the fundamental problem patients and physicians have as a result of the excessive PA demands by insurers. MSSNY will continue to aggressively support legislation to address PA hassles. This includes legislation to prohibit repeat prior authorization requirements for the same treatment, for the same patient, once initially authorized by a health insurer, and legislation to prohibit health insurance plans from applying PA requirements to physicians who have received at least 90% approval from an insurer for prior authorizations for a specific treatment. Furthermore, any legislation should ensure payment for delivering these services.
Increased Penalties for Failure to Follow Laws. MSSNY will continue to push for stronger DFS and DOH enforcement against health insurers that engage in patterns of inappropriately delaying payment for patient care delivery. This often occurs through the excessive and unnecessary medical record review demands. In 2023, DFS imposed $120 million in recoveries for violations of the State’s Prompt Payment law. However, it is outrageous that physicians and other care providers must continue to regularly resort to governmental intervention to be paid fairly for delivering appropriate patient care. Practice transactional costs are often immense, with hours per day spent on unnecessary phone calls and e-mails to health insurance bureaucrats, solely to ensure that patient care is appropriately compensated.
New York’s Prompt Payment law, enacted over 25 years ago, needs to be updated to increase the penalties and interest that can be imposed on health insurers for illegally delaying payment for health care claims that should be paid pursuant to enrollees’ contract with their health insurer. Furthermore, MSSNY supports
increased funding to DFS so that the agency can hire more enforcement staff to help ensure that complaints regarding health insurer delay tactics be promptly investigated and remedied.
Enhancing Network Adequacy. To ensure the availability of comprehensive physician networks and protect against unfair narrowing of these networks MSSNY supports legislation which would provide due process protections for physicians whose contracts are not renewed by insurance companies.
Furthermore, to enhance patient access to timely care, reforms should be enacted to: improve old standards that DFS and DOH use to determine network adequacy; adopt comprehensive standards to meet the health needs of all covered insureds including those in diverse and underserved communities across New York; improve transparency, so consumers understand the scope, scale, and quality of the network to be able to comparison shop; and increase regulatory oversight of incorrect participating physician lists.
Enhancing Insurance Coverage. MSSNY supports efforts to enhance the availability of affordable, comprehensive health insurance coverage for our patients. This includes limiting often exorbitant out-of-pocket costs, such as coinsurances and deductibles, for private commercial health plans and improving benefit designs and subsidies for patients with Medicaid and policies purchased through New York State’s Health Insurance Marketplace. It should also include enhancing payment for various public health insurance programs, which contain some of the lowest reimbursement rates in the country.
Revising New Payment Consent Requirements. A new policy adopted during the 2024-25 State Budget requires physicians to separately obtain patients’ consent for payment distinct from the consent for treatment.
The most pressing concern with the requirement is that physicians must obtain consent for payment after the delivery of services, not before, which is inconsistent with state and federal laws that require the disclosure of charges prior to the delivery of services. It also presents the unreasonable possibility that the physician may not get compensated by the patient if the patient refuses or is unable to sign the form, after care is provided. MSSNY is urging the Legislature, the Department of Health, and the Governor to revise this requirement in the 2025 Legislative Session.
Increasing Inadequate Payments for Public Insurance Programs. With nearly 30% of New York’s population receiving health insurance coverage through various public programs such as Medicaid, Essential Plan or CHIP, MSSNY will continue to advocate for increased payments from these programs, including restoration of payments from New York State to cover the coinsurance for patients who are dually covered by Medicaid and Medicaid. While there have been some steps taken in recent State Budgets to provide modest increases to Medicaid payments, New York continues to have one of lowest Medicaid fee schedules in the country when compared to Medicare fees.
The low reimbursement by these programs has a significant deterring impact on the number of patients covered by these programs that a physician office can realistically handle and remain financially sound keeping their offices open and available for patient care. The reimbursement is often below the cost of actually providing the care to a patient. With the growing awareness of cost increases that can occur when hospitals purchase community physician practices, it is imperative that policymakers work to provide fair payment for public programs that would help enable physicians to remain independent community care providers.
Questions Regarding The New York Health Act. While MSSNY recognizes there may be some merit for the creation of a single payor health insurance plan for New York State, we also believe it is critically important for the State to undertake a thorough “real world” analysis of the strengths and weaknesses of any such proposal.
An analysis would need to address the following questions:
- Will access to patient care be impacted by prior authorization and other administrative hassles associated with providing needed patient care?
- Will there be a fair payment methodology that incentivizes physicians to stay to deliver care in New York rather than exacerbate the many other practice environment factors that are causing physicians to retire early or re-locate to other more physician-friendly states?
We appreciate that versions of this legislation have attempted to provide some clarity to these questions.
However, there have been numerous instances over the past several years where the medical community has had to strenuously advocate to prevent a patient access to care crisis by fighting the implementation of proposed steep Medicare and Medicaid cuts, in response to Federal and State Budget shortfalls. It is certainly foreseeable that a similar situation could occur under a single payer system, and it is imperative that these concerns be addressed as part of any single payer proposal.
PHYSICIAN WELLNESS
The Physicians Foundation’s 2024 Survey of America’s Current and Future Physicians showed that 60% of physicians and residents and 70% of medical students reported often experiencing burnout. More than half of physicians know of a physician who has ever considered, attempted, or died by suicide. For years, physicians have become increasingly demoralized by the systemic stressors that have fueled the burnout crisis in healthcare. Factors include increasing regulatory requirements, administrative and record keeping burdens, documenting unproven measures, and liability issues, resulting in growing work hours and time in front of a computer screen instead of interacting with patients. Seven in ten physicians and medical students, and at least six in ten residents agree that consolidation is having a negative impact on patient access to high-quality, cost-efficient care. According to physicians, the negative impacts of mergers/acquisitions include job satisfaction (50%), quality of patient care (36%), independent medical judgment (35%) and patient healthcare costs (30%). For the third year in a report, stigma and structural barriers prevent current and future physicians from seeking mental health care.
Physician burnout has been linked to lower productivity, absenteeism, medical errors, and less effective healthcare teams. For the benefit of our health care system and our patients, policymakers must find ways to reduce the contributing factors to physician burnout.
Promote Peer Support (MSSNY P2P)
MSSNY has implemented a Peer-to-Peer (P2P) program for physicians that offers an opportunity to talk with a peer about some of life’s stressors. The MSSNY P2P program allows trained peer supporters to assist their colleagues who need help in dealing with work, family stressors, and COVID-19. To further enable its P2P program, MSSNY supports legislation to facilitate the ability of physicians to have these therapeutic “peer-to-peer” conversations by providing confidentiality protection for organizations and individuals that provide physician peer support, like protections provided to the NYS Bar Association peer support activities. MSSNY actively advocates for the continued funding of the Committee for Physician Health, founded to help physicians affected by substance
abuse, addiction, mental health problems, and cognitive disorders.
CONTAINING EXORBITANT MEDICAL LIABILITY COSTS
Our patients depend upon having access to their community-based physicians as well as a regional healthcare safety net. As our healthcare system continues to face enormous cost pressures including annual Medicare cuts and pervasive insurer tactics to delay payment for care, it is imperative to protect our system from de-stabilizing cost increases that further impair hospitals and physicians’ ability to deliver the care needed and expected by our patients.
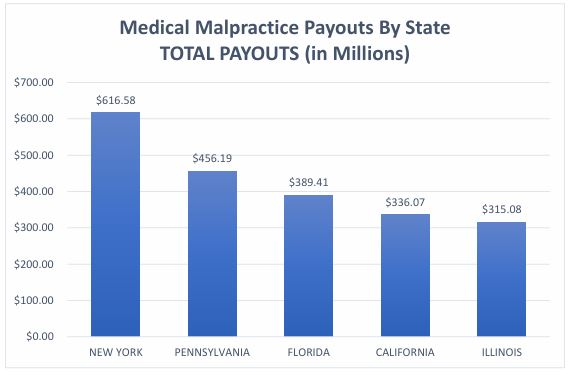
The most significant cost pressure continues to be New York’s notoriously excessively high liability costs, which far exceed any other state in the country, including more populous states such as California and Texas. For these reasons, New York is perennially ranked among the worst states in the country for physicians to practice medicine.
Despite the dire need for reduction in these costs, the Legislature has done the opposite, passing legislation in each of the last 3 years to greatly expand damages awardable in a wrongful death action. In January 2023 and again in December 2023, Governor Hochul importantly vetoed this legislation, which if enacted would have necessitated premium increases of nearly 40%. The Governor identified several reasons for vetoing these bills, including that it “would increase already high insurance burdens on families and small businesses and further strain already-distressed healthcare workers and institutions” which would be “particularly challenging for struggling hospitals in underserved communities.”
 She also raised concerns regarding the “significant unintended consequences” of this proposal, including the impact to our community healthcare infrastructure because of the likely huge increase in liability costs the legislation would incur through the anticipated expanded liability awards.
She also raised concerns regarding the “significant unintended consequences” of this proposal, including the impact to our community healthcare infrastructure because of the likely huge increase in liability costs the legislation would incur through the anticipated expanded liability awards.
However, instead of developing a comprehensive bill that addressed concerns on both sides of the issue, the State Legislature passed yet another one-sided version of this bill in 2024. MSSNY with numerous other allies continue to urge that any legislation to expand liability should only be considered in the context of a comprehensive effort to address New York’s excessive liability costs. While many other states have passed laws to contain medical liability payouts and provide greater fairness in medical liability litigation, New York has not, which is why our medical liability insurance and payout costs far exceed every other state in the country. In fact, in 2023 New York exceeded the 2nd highest state Pennsylvania by 35%, the 3rdhighest state Florida by 58%, and 4th highest state California by 83%! The Legislature must take steps to contain these costs.
Measures to reduce our liability cost pressures that MSSNY Supports include:
- Meaningful Certificates of Merit. New York’s existing weak or inadequate Certificate of Merit requirement should be expanded to require a more detailed justification be provided for filing a medical malpractice lawsuit. This is particularly important given that roughly 2/3 of all medical liability actions result in no payment to the plaintiff, yet tens of millions of dollars are spent on defense costs, each year, for these non-meritorious claims.
- Expert Witnesses Who are Peers. An expert witness in a medical malpractice action should be required to practice in the same specialty as the defendant physician.
- Limiting Exorbitant and Arbitrary Damages. MSSNY supports placing reasonable limits on non-economic damages, as have over other 30 other states across the country.
- Providing Alternative Resolution Venues. MSSNY supports creating alternative systems for resolving liability claims such as medical courts or a Neurologically Impaired Infants Fund.
- Reducing interest rates on court judgments from 9% to a market-based rate.
- Protecting Availability of Comprehensive Malpractice Coverage. MSSNY strongly supports continuing an adequately funded Excess Medical Malpractice Insurance Program without imposing unfair cost-sharing requirements on physicians receiving this essential coverage.
In addition to the opposing the wrongful death liability expansion bill, MSSNY:
- Opposes Anti-Consumer Attorney Fee Increases. MSSNY opposes the elimination of consumer protections against exorbitant attorney contingency fees in medical liability actions.
- Opposes Pre-Trial Cost-Sharing. MSSNY opposes proposals that would force litigants in multi-defendant actions to make decisions before trial regarding post-verdict cost-sharing.
- Opposes the Awarding Pre-Judgment Interest. MSSNY opposes legislation that would permit awarding the interest prior to a final judgment in a civil action.
Protecting Care Improvement Efforts through Peer Review. MSSNY continues to support efforts to enhance quality improvement by encouraging open dialogue in hospital peer review proceedings without fear that such statements may be used against them in litigation. There is an absurd exception to New York’s peer review confidentiality law that permits the discovery by trial lawyers of statements by a physician who subsequently is sued. This long-standing problem was further exacerbated by a recent 2d Department decision (Siegel v. Snyder) that further limited the confidentiality of all peer review discussions where the identity of the speaker cannot be discerned. Because New York’s excessive liability environment discourages open communication of health care delivery, confidentiality of efforts to learn from adverse events in care delivery is essential. To address this problem, MSSNY supports legislation to ensure that peer review discussions can be robust without fear of litigation by ensuring its confidentiality.
PROTECTING PATIENTS THROUGH PRESERVING PHYSICIAN-LED TEAM CARE
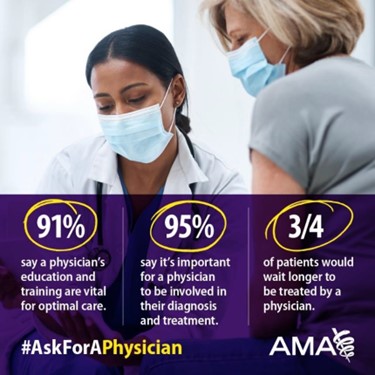
To ensure our patients receive the highest quality care, MSSNY supports efforts to preserve physician-led team care in health care settings across the state. Not only is it best for care quality, but it is also what patients want. A recent national survey reported that 95% of patients believe it is important that a physician be involved with their diagnosis and treatment decisions.
We agree that many regions of the state face a lack of critically needed physicians. But efforts to address these gaps must begin by focusing on affirmative steps that can be taken to address the shortage of physicians rather than seeking to replace them. This includes increasing medical student loan repayment programs, increasing funding for rural residency spots, expanding clinical locations for appropriately trained “limited permit” IMG physicians, and increasing woefully inadequate Medicaid reimbursements.
We are very concerned with the adverse patient impact of completely removing the important oversight and coordination role which a trained physician plays in overseeing a patient’s care, particularly as it relates to the ordering of diagnostic tests, the evaluation of the effectiveness of various prescription medications and treatments and the ongoing assessment of the patient’s response to treatment. All of these oversight functions are essential safeguards in assuring that lesser trained professionals do not overlook important elements of the patient’s unique circumstances.
Training. It is impossible to overstate the importance of a physician’s comprehensive education and training to ensuring quality patient care. Most physicians must complete 4 years of medical school plus 3-7 years of residency and fellowships, including 10,000-16,000 hours of clinical training before they are permitted to treat patients independently. During this training physicians receive approximately 5,000 hours of clinical experience in medical school, 4,000 hours of clinical experience in internship, and 6,000 to 18,000 clinical hours during specialty training. This extensive training makes physicians best suited to deliver and coordinate needed primary and specialized patient care.
The Cost-Effectiveness of Physician-Led Team Care. Expanding scopes of practice will not be the panacea some assert. Multiple studies show that when non-physicians are permitted to practice independently, this difference in training presents patient safety risks and increases health care costs. One study of PA and NP care found that care provided to patients exclusively by non-physicians (PAs and NPs) was much more expensive than the care delivered by physicians because these non-physician providers ordered more tests and referred more patients to specialists and hospital emergency departments than physicians did. The care provided by non physicians was also determined to have lower quality rankings. Another study of NPs in the Emergency Departments reported that NPs delivering emergency care without physician supervision or collaboration in the Veterans Health Administration (VHA) increase lengths of stay by 11% and raise 30-day preventable hospitalizations by 20% compared with emergency physicians.
Legislation. It is imperative that the public have detailed information regarding the various health care providers from whom they are or are considering receiving treatment. To that end, MSSNY supports “Truth in Advertising” legislation that would ensure that all health care providers be required to conspicuously identify their type of state license when treating patients in all health care settings and in advertisements, particularly when they identify themselves as a “doctor.”
MSSNY Opposes legislation that would remove the important oversight provided by a trained physician in delivering patient care, including by:
- Inappropriately permitting CRNA independent practice.
- Inappropriately permitting independent practice by PAs and permitting them to perform fluoroscopy without appropriate supervision.
- Inappropriately expanding the authority of NPs to deliver care without collaboration by physicians practicing in the same specialty as the NP.
- Inappropriately expanding the ability of podiatrists to treat up to a patient’s knee.
- Inappropriately permitting pharmacists to order and conduct patient lab tests without physician coordination.
- Inappropriately granting psychologists prescribing privileges.
- Inappropriately granting the ability of optometrists to perform surgery.
At the same time MSSNY supports the ability of otolaryngologists to dispense hearing aids at fair market value. With the federal government authorizing the sale of hearing aids over the counter, there is no logical reason to maintain an artificial distinction between which providers can sell hearing aids at fair market value.
Our patients deserve care delivered by or coordinated with a highly trained physician. We believe enhancing the practice environment for physicians in New York, instead of replacing them with non-physician providers, is a much more viable and practical strategy to promote patient safety, ensure access to care, and to control costs. ion between which providers can sell hearing aids for profit.
PROMOTING PUBLIC HEALTH
Reproductive Health
Reproductive health care, including access to birth control and safe and legal abortion care, is an essential part of health and well-being. While Roe v. Wade was overturned, abortion remains legal in New York State. Preserving the right for women to have access to reproductive and sexual health care services remains essential. Abortion has been legal under New York State law since 1970 – three years before the Roe v. Wade decision. MSSNY is strongly opposed to any federal or state legislation that would prohibit physicians from exercising clinical judgment in the delivery of medical care and strongly supports New York State protections for physicians from legal sanctions for providing needed patient care, legal in New York but potentially illegal in other states.
MSSNY supports measures to protect practitioners licensed and residing in New York from legal or personal liability when delivering healthcare services to residents of New York State or any other state, whether in person or via telemedicine, when the services provided comply with New York State laws and regulations. MSSNY supports legislation to provide protections, including against extradition to any other state, for providers who perform comprehensive women’s health services that are legal in New York State. MSSNY supports legislation that allows anyone sued in another state for providing or helping someone access reproductive health services in New York to file their own legal action for unlawful interference with a protected right, and to recover damages from the out of state litigant.
Additionally, ensuring access to reproductive health services medications should continue to fall under the FDA’s authority to determine whether drugs are safe and effective. MSSNY also supports legal efforts to ensure that mifepristone and misoprostol are available to anyone for whom they are prescribed and will support efforts to ensure that both these medications continue to be available, and that the FDA retain its regulatory authority. MSSNY supports legislation and other efforts to expand access to emergency contraception, including making emergency contraception more readily available, and will continue to support sexual health education programs amongst adolescents.
End of Life Care
At the MSSNY 2024 House of Delegates, members rescinded its previous position on assisted suicide and euthanasia. MSSNY policy now supports legislation such as the medical aid in dying act and that physicians should continue to retain their choice to opt-in or decline to engage in the processes and procedures as outlined in any proposed medical aid in dying legislation.
Challenging decision-making concerning end of life care has increased the burden on physicians, patients, and family members. To address these challenges, MSSNY seeks, among other items, the development of a state central depository for eMOLST (Medical Orders for Life Sustaining Treatment) form; adequate reimbursement for end-of-life care and expanded options for obtaining long-term care insurance. MSSNY also recognized that end of life care, including access to hospice care, is a human right.
Promoting Immunizations
MSSNY continues to aggressively promote the importance of immunizations. Vaccines have reduced and, in some cases, eliminated, diseases that killed or severely disabled people just a few generations ago. It is not an overstatement to say that immunization protects future generations. For example, Smallpox has been eradicated because of vaccine. Vaccinations against rubella has dramatically decreased the risk that pregnant women will pass this virus on to their fetus or newborn. Vaccines are safe and effective—and they save lives.
 In 2019, MSSNY together with many other groups supported a law to require every child attending a public, private, or parochial school to receive the appropriate immunizations, except when it is medically contraindicated. However, there has seen an increase in the number of medical exemptions issued to school- age children from vaccination requirements. MSSNY has strongly encouraged physicians to follow the CDC guidance when issuing a medical exemption and has reminded that falsely certifying a medical exemption form could result in a disciplinary action. MSSNY will continue to ensure that there are only medical exemptions for the school requirement.
In 2019, MSSNY together with many other groups supported a law to require every child attending a public, private, or parochial school to receive the appropriate immunizations, except when it is medically contraindicated. However, there has seen an increase in the number of medical exemptions issued to school- age children from vaccination requirements. MSSNY has strongly encouraged physicians to follow the CDC guidance when issuing a medical exemption and has reminded that falsely certifying a medical exemption form could result in a disciplinary action. MSSNY will continue to ensure that there are only medical exemptions for the school requirement.
MSSNY continues to support state funding for a public health campaign to promote immunizations to educate the public about the importance of vaccinations. MSSNY also supports requiring all public, private, and parochial schools in New York State and New York City to report immunization rates and medical
exemptions to one central NYS Department of Health database, to help effectively track immunization rates throughout the state. MSSNY supports universal reporting of adult immunizations to the New York State Immunization Information System (NYSIIS), either directly or via health information exchanges and supports removing the requirement for patient permission to report adult vaccines to the registry.
Preventing and Responding to Infectious Disease Outbreaks
MSSNY’s Committee on Emergency Preparedness and Disaster/Terrorism Response continues to educate physicians and the healthcare community on how they best can work with the State’s public health infrastructure to prevent the spread of infectious diseases. Certainly, the COVID-19 pandemic and recent natural disasters have reminded us of the need to prepare and respond appropriately to any type of infectious disease outbreak.
Substance Use Disorders
In New York State, a recent report showed that the number of filled opioid analgesic prescriptions declined from more than 9 million in 2013 to under 6 million in 2022 – a 42.1% decrease over 10 years. This result is in large part due to the pervasive use by physicians and other providers to of the State’s Prescription Monitoring Program Registry (PMP) to prevent “doctor-shopping”. Even with this profound change in prescribing, the Legislature has imposed numerous additional often burdensome requirements on prescribers, including mandatory electronic prescribing, mandatory pain management CME, limiting the duration of initial opioid prescriptions for acute pain, a required a written treatment plan when prescribing opioid medications in cases of long-term opioid use and chronic pain, and mandatory consideration of alternatives to opioid medications prior to prescribing.
The 2022 Centers for Disease Control and Prevention’s (CDC) Clinical Guideline for Prescribing Opioids for Pain, while focusing on strategies for mitigating risks when prescribing opioids including an emphasis on the use of nonpharmacologic and nonopioid therapies, also showed that physicians and patients are making more informed treatment decisions when it comes to pain management. Since 2016 MSSNY has provided a pain management course for physicians and thousands of physicians have taken this course. In 2025, MSSNY will begin a refresher course on the use of the PMP registry as a tool to help ensure physicians are fully aware of their patient’s controlled substance use history. Furthermore, MSSNY actively works to increase physician and patient awareness to combat
the opioid and pain crisis and supports efforts to expand access to MAT medications for addiction treatment, including methadone for patients with opioid use disorders.
Minimizing Community Health Impact of Hospital Closures
The closure of hospitals or diminution in services offered by these institutions has a significant adverse impact on access to care for the patients that live in the communities served by these hospitals. It also creates significant additional pressures on already-stretched surrounding facilities that must take on treating a significant number of additional patients, particularly problematic when these institutions already face staffing shortages which contribute to long emergency department wait times. Understanding the downstream health care system impact of hospital closures, the MSSNY House of Delegates recently adopted a position calling upon MSSNY to advocate that there be “meaningful local physician and patient input into proposals to close, downsize or re-purpose
hospitals that could adversely impact health care options in communities served by those hospitals”. In this regard, MSSNY supports legislation to ensure appropriate advance notification to communities prior to the proposed closure, downsizing or repurposing of hospitals, including public hearings in those communities affected by such closures, downsizing or re-purposing.
Health Equity
MSSNY adopted a statement developed by the MSSNY Committee on Health Equity that says in part that MSSNY affirms that racism is a public health crisis and that MSSNY’s mission statement will be evaluated to ensure that it supports equity in all aspects of its work. Furthermore, MSSNY will systematically evaluate its policies and procedures to be clear that it supports equity in all aspects of its work, in both existing and in future policies and procedures, and that records of this process will be visible to all members. MSSNY, through its Committee on Health Equity will seek to:

- Increase awareness of how discrimination based on factors such as racism, classism, cisgenderism, heterosexism, ableism, patriarchy, and xenophobia contribute to both societal and health inequities and to ensure that all New Yorkers receive the best care possible and can achieve the best health possible.
- Work with stakeholders, including the AMA, specialty societies, Albany leadership, community groups, and others to eliminate inequities, particularly those inequities that adversely impact the health and well-being and access to and quality of care for persons who are from historically disadvantaged populations.
- Prevent and manage diseases that are prevalent in historically disinvested populations burdened with poorer disease outcomes, including diabetes, hypertension, and cancer, through educational programming for physicians and other stakeholders.
MSSNY will also advocate for fair payment for treatment of such conditions. - Reverse the troubling increases in race/ethnic based health inequities such as maternal mortality; promote expanded funding for programs that attract a more diversified physician workforce; and increase the number of minority faculty and faculty with disabilities teaching in medical schools. MSSNY will also work to expand medical school pipeline programs in rural and urban areas to address the shortage of physicians in medically underserved areas of New York.
- Support gender affirming care by advancing the ability of physicians in New York to provide gender affirming care and opposing the criminalization of providing gender affirming care for youth.



