Let’s Defend the Practice of Medicine and the Patients We Serve
Friday, May 30, 2025

Let’s Defend the Practice of Medicine and the Patients We Serve
Colleagues:
Your elected leadership and staff are fully engaged as we approach the final stretch of the New York State Legislative Session. Simultaneously, we are preparing for the upcoming American Medical Association House of Delegates and actively participating in the outstanding events hosted by our county medical societies.
State-Level Advocacy
At the state level, our advocacy efforts have intensified in response to numerous legislative challenges. To address the problematic financial consent requirements enacted last year but put on hold by the Health Department, we are working closely with key legislators on new legislation to fix this problem, while opposing bills such as S.6375-A that would impose excessive administrative burdens.
We are also disappointed that S4423 passed the Senate by a vote of 51–10 and has now moved to the Assembly. This legislation has been linked to a 40% increase in medical liability insurance premiums for physicians. The bill has not yet passed the Assembly, but if it does, we will continue to urge Governor Hochul to veto this bill—as she has done in the past three years. However, in this election year, the outcome remains uncertain. We strongly encourage you to use our grassroots advocacy tools to send a letter to your Assembly member opposing S4423/A6063: OPPOSE Latest Wrongful Death Bill and Preserve Patient Access to Healthcare
Federal-Level Concerns
On the federal front, the recently passed House reconciliation bill—referred to as the “Big, Beautiful Bill”—has created further uncertainty. We support key provisions including:
- Removing Medicare from MACRA and eliminating the flawed budget neutrality requirements
- Tying physician payment updates to the Medical Economic Index at 100%, not the proposed 10%
We urge all physicians to sign the grassroots letter to communicate these priorities to lawmakers: MSSNY Urges Congress to Increase Medicare Payments and Oppose Deep Cuts to Medicaid
Additionally, we are monitoring developments within the Department of Health and Human Services. A recent vaccine announcement via Twitter, bypassing the traditional review process, has caused widespread concern. The proposal to eliminate coverage of COVID-19 vaccination during pregnancy, under the so-called “Making America Healthy Again” initiative, is not only dangerous but threatens to undermine decades of progress in vaccine trust and coverage. With the potential expiration of North America’s 25-year measles elimination status, this action is both irresponsible and reckless.
MAHA Report Misrepresentation
As an otolaryngologist, I find the MAHA Report’s recent statements on common surgical procedures deeply troubling. The report asserts that:
Adenotonsillectomy for children with sleep apnea, a historically common procedure, conferred no benefit in trials—suggesting the many, and often severe, harms of this surgery are unnecessary. Tympanostomy tubes for recurrent ear infections, despite being recommended by professional societies, did not reduce infections in trials—showing common surgeries cause harm without offering benefits. These sweeping claims are based on single studies with methodological flaws. The adenotonsillectomy claim is drawn from a trial involving 141 children with only mild sleep apnea, using tools that did not assess executive functioning—a key impact area of the condition. The tympanostomy analysis stems from a study in which only 250 of 1,329 identified patients were randomized, and many in the control group still received surgical intervention, undermining the integrity of the data. One trial does not equate to “trials”, patient preference is not randomization, and poorly supported conclusions are still just that—sloppy.
Stay Engaged
MSSNY continues to advocate fiercely on your behalf, at both the state and federal levels. These are complex and pivotal times for the practice of medicine. Your engagement is critical. Support our efforts by contributing to MSSNYPAC.org, and please take action through our grassroots advocacy network.
Together, we can defend the practice of medicine and the patients we serve.
All the best,
David Jakubowicz, MD, FACS
MSSNY President

Telehealth Use Varies Widely by Condition, Study Finds
A new study published in JAMA Network Open offers critical insights into how the diagnosis at hand influences whether a primary care visit is conducted in person, by phone, or via video. Researchers examined over 7.5 million primary care encounters across the Veterans Health Administration from March 2020 to September 2021, one of the largest analyses of its kind. The study found that telehealth adoption wasn’t just influenced by demographics or digital access—it was most strongly associated with clinical conditions.
In-person visits were predominant (60.7%) and remained essential for managing chronic diseases requiring physical exams, lab work, or detailed assessments, such as diabetes, COPD, and asthma. Conversely, video visits were used more frequently for conditions where physical mobility is limited or where patients face barriers to clinic attendance, such as dementia, HIV, Parkinson’s disease, and behavioral health diagnoses like PTSD. Telephone visits, while widely used early in the pandemic, were more common for acute, low-complexity concerns or when patients lacked the capability for video.
Importantly, the study also observed geographic and racial disparities in modality of use. Patients in rural areas and Black patients were less likely to have video visits, raising concerns about digital health equity. However, after adjusting for diagnosis, much of the variation in telehealth modality was explained by clinical need rather than patient preferences or demographics.
Variability in Primary Care Telehealth Delivery Methods Across Chronic Conditions (Jacqueline M. Ferguson, PhD; Liberty Greene, MS; James Van Campen, MS, JAMA, 3/26).
Transforming Healthcare Payments: Lessons from the Financial Sector
As healthcare costs rise and patient expectations evolve, providers face increasing pressure to modernize the payment experience. A recent opinion piece published in MedCity News argues that healthcare must take cues from the financial services industry to meet modern consumer demands for seamless, flexible, and trustworthy payment systems. Drawing from two decades in finance before transitioning to healthcare, the author highlights how consumer behavior has driven payment innovation, particularly through frictionless, multichannel solutions like digital wallets and peer-to-peer apps.
However, electronic health records (EHRs) and rigid payment infrastructure have lagged in healthcare. Patients, especially younger generations, increasingly expect the same effortless experiences they enjoy with major retailers. The article urges providers to integrate diverse payment options—cards, bank transfers, digital wallets—directly into patient portals and to maintain visual and functional consistency to build trust.
Unlike retail, healthcare spending is often non-discretionary, amplifying the emotional and financial toll of poor billing experiences. Providers can support affordability while enhancing patient satisfaction by offering structured payment plans and improving interface design.
Bridging Financial Services and Healthcare (Welch, MedCityNews, 5/13).
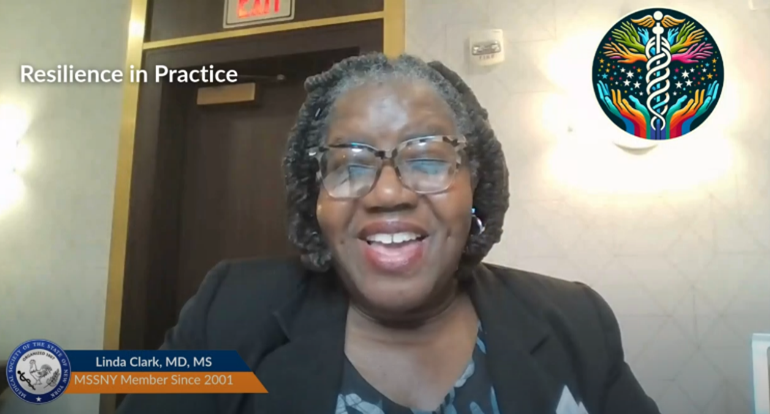
Dr. Linda Clark on Building Trust and Equity Through Shared Experience
In this week’s Resilience in Practice feature, Dr. Linda Clark, a respected MSSNY member and physician leader, reflects on how her identity as a Black physician strengthens her ability to build trust and foster healing. Through shared experience and cultural understanding, Dr. Clark creates space for more meaningful patient relationships and helps bridge persistent gaps in healthcare equity.
Her story is a reminder that empathy isn’t just a trait; it’s a clinical asset. Dr. Clark’s leadership uplifts her community while modeling how New York physicians can deepen their impact through connection, representation, and advocacy.
MSSNY proudly features Dr. Clark as part of our continued commitment to highlight underrepresented voices in medicine. Join our Minority Affairs Section to support and elevate colleagues dedicated to reshaping the future of care.
Physician Wait Times Surge Amid National Doctor Shortage
A new analysis from AMN Healthcare underscores a critical strain on the U.S. healthcare system: longer wait times for physician appointments are emerging as a clear signal of a growing physician shortage. Across 15 major metropolitan areas, patients now wait an average of 26 days to see a new physician, up 8% from 2022 and 24% from 2017. In particular, wait times for family medicine rose 30% over the past year. The report attributes these delays to several compounding factors, including physician burnout, retirements, and a slower pipeline of new medical professionals.
The implications for physicians are clear: overburdened schedules, rising patient demand, and increased pressure on practice efficiency. MSSNY continues to advocate for policy solutions that support physician well-being and career longevity.
2025 Survey of Physician Appointment Wait Times and Medicare and Healthcare Technology Medicaid Acceptance Rates (AMN Healthcare, 5/2025).
The Yankees are Back with Healthcare Appreciation Part 2!
Dates: August 25th-27th
All tickets come with a $15 meal/drink vouchers and a choice between Tumbler or Scrub Top.

Explore the Future of Occupational Medicine at the 2025 MARCOEM Conference
The 2025 Mid-Atlantic Regional Conference on Occupational and Environmental Medicine (MARCOEM) returns October 25–26, hosted at Johns Hopkins University’s Bloomberg Center in Washington, D.C. Co-chaired by Dr. Hasan Nezam and Dr. Jeffrey Jacobs, the conference will address critical topics including AI in medicine, toxicology updates, pregnancy in the workplace, and corporate health strategies from industry leaders like Disney and Bristol Myers Squibb.
Register Now | View Flyer here.

Capital Update May 30, 2025
- Prior Authorization Reform Legislation Advances in Both Houses – Please Continue Efforts to Urge Passage
- Senate Again Passes Disastrous Liability Expansion Bill – Please Urge Your Assembly Members to Oppose
- Physician Due Process Bill Advances
- House of Representatives’ Reconciliation Package on Medicaid & Medicare Passes Full House; Now Headed to the Senate
- Legislation Passes to Provide Coverage for Lung Cancer Follow-Up Testing
- Queens Physician Leaders Join Senator Liu to Urge Passage of Legislation to Expand Coverage for Diabetes Screening

Veterans Matters CME Webinar
Join us for the eighth session of the Veterans Matters eight-part webinar series, dedicated to supporting the mental health and well-being of veterans. This session, PTSD in Returning Veterans, will be held on June 4, 2025, at 07:30 AM and led by Frank Dowling, MD.
In this session, you’ll gain valuable insights into the educational objectives:
- Identify diagnostic criteria for PTSD.
- Discuss medical and psychiatric comorbidities of military-related PSTD.
- Discuss evidence-based treatment modalities for PTSD, including medications and psychotherapy.
- Discuss strategies to help veterans overcome stigma to seek and accept treatment for military-related trauma.
Register now to reserve your spot.
The Medical Society of the State of New York is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
The Medical Society of the State of New York designates this live activity for a maximum of 1.0 AMA PRA Category 1 credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Medical Matters: Infectious Diseases & Disasters
Tuesday June 17th – 7:30-8:30am
There are myriad considerations to account for when preparing for disasters. Infectious diseases that can accompany a variety of disaster situations should be at the forefront of everyone’s preparedness learning. Learn more about the relationship between infectious diseases and disasters by registering for the next Medical Matters webinar, Infectious Diseases and Disasters, on June 17th at 7:30am. William Valenti, MD chair of MSSNY Infectious Diseases Committee will serve as faculty for this webinar.
Educational Objectives are:
- Outline possible infectious disease proliferation during various types of disasters
- Review recommendations for protections for responders and residents in disaster areas
- Describe best practices to avoid vaccine preventable diseases (VPD) during disasters
- Examine the impacts of climate on disasters and resultant infectious diseases
Additional information or assistance with registration may be obtained by contacting Melissa Hoffman at [email protected]
The Medical Society of the State of New York is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
The Medical Society of the State of New York designates this live activity for a maximum of 1.0 AMA PRA Category 1 credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
The Evolution of Artificial Intelligence (AI) in Medicine: Historical Insights, Current Applications, and Future Trends
Wednesday June 25th – 7:30-8:30am
Artificial Intelligence (AI) has seemingly evolved at breakneck speed and while the beneficial applications for AI in medicine are undeniable, it is important to maintain perspective and understand the best ways in which AI can benefit the practice of medicine. Donald E. Moore, MD, chair of MSSNY AI Taskforce will serve as faculty for this session, The Evolution of Artificial Intelligence (AI) in Medicine: Historical Insights, Current Applications, and Future Trends.
Educational objectives:
- Examine AI Fundamentals
- Recognize Current Applications of AI in Medicine
- Foster Critical Thinking and Continuous Learning
- Develop Practical Skills for AI Integration
The Medical Society of the State of New York is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
The Medical Society of the State of New York designates this live activity for a maximum of 1.0 AMA PRA Category 1 credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Secure Your Financial Future with MSSNY’s Physician Life Income Plan (PLIP) Informational Webinar
On June 12, join us in discussing the Physician Life Income Plan (PLIP) as a premier member benefit, spotlighted in Forbes and MD News for their approach to retirement planning. PLIP is a tailored financial solution that empowers physicians to maximize tax-deferred growth, enjoy tax-free withdrawals, and protect assets from creditors — all while bridging the retirement gap with unparalleled flexibility and security.
With no contribution limits or early withdrawal penalties, PLIP stands apart from traditional retirement plans. Members can reallocate current investments, such as cash, CDs, or cash value life insurance, into a tax-advantaged vehicle that offers over 80 investment allocation options, including indexes like the S&P 500. All funds in PLIP grow tax-free, are withdrawn tax-free, and pass to beneficiaries tax-free.

Streamline Your Payment Process with CardConnect
MSSNY members gain exclusive access to secure, cost-effective payment solutions tailored to healthcare practices. Enjoy optimized rates, next-day funding, and dedicated 24/7 support. Simplify your operations today. Connect with Our Payment Expert Mark Bristow 914.506.1984